Abstract
Kidney stone disease is a crystal concretion formed usually within the kidneys. It is an increasing urological disorder of human health, affecting about 12% of the world population. It has been associated with an increased risk of end-stage renal failure. The etiology of kidney stone is multifactorial. The most common type of kidney stone is calcium oxalate formed at Randall’s plaque on the renal papillary surfaces. The mechanism of stone formation is a complex process which results from several physicochemical events including supersaturation, nucleation, growth, aggregation, and retention of urinary stone constituents within tubular cells. These steps are modulated by an imbalance between factors that promote or inhibit urinary crystallization. It is also noted that cellular injury promotes retention of particles on renal papillary surfaces. The exposure of renal epithelial cells to oxalate causes a signaling cascade which leads to apoptosis by p38 mitogen-activated protein kinase pathways. Currently, there is no satisfactory drug to cure and/or prevent kidney stone recurrences. Thus, further understanding of the pathophysiology of kidney stone formation is a research area to manage urolithiasis using new drugs. Therefore, this review has intended to provide a compiled up-to-date information on kidney stone etiology, pathogenesis, and prevention approaches.
1. Introduction
1.1. Overview of Kidney Stones
Kidney stones are mainly lodged in the kidney(s) [1]. Mankind has been afflicted by urinary stones since centuries dating back to 4000 B.C. [2], and it is the most common disease of the urinary tract. The prevention of renal stone recurrence remains to be a serious problem in human health [3]. The prevention of stone recurrence requires better understanding of the mechanisms involved in stone formation [4]. Kidney stones have been associated with an increased risk of chronic kidney diseases [5], end-stage renal failure [3, 6], cardiovascular diseases [7, 8], diabetes, and hypertension [9]. It has been suggested that kidney stone may be a systemic disorder linked to the metabolic syndrome. Nephrolithiasis is responsible for 2 to 3% of end-stage renal cases if it is associated with nephrocalcinosis [10].
The symptoms of kidney stone are related to their location whether it is in the kidney, ureter, or urinary bladder [11]. Initially, stone formation does not cause any symptom. Later, signs and symptoms of the stone disease consist of renal colic (intense cramping pain), flank pain (pain in the back side), hematuria (bloody urine), obstructive uropathy (urinary tract disease), urinary tract infections, blockage of urine flow, and hydronephrosis (dilation of the kidney). These conditions may result in nausea and vomiting with associated suffering from the stone event [12]. Thus, the treatment and time lost from work involves substantial cost imposing an impact on the quality of life and nation’s economy.
1.2. Epidemiology of Kidney Stones
Globally, kidney stone disease prevalence and recurrence rates are increasing [13], with limited options of effective drugs. Urolithiasis affects about 12% of the world population at some stage in their lifetime [14]. It affects all ages, sexes, and races [15, 16] but occurs more frequently in men than in women within the age of 20–49 years [17]. If patients do not apply metaphylaxis, the relapsing rate of secondary stone formations is estimated to be 10–23% per year, 50% in 5–10 years, and 75% in 20 years of the patient [15]. However, lifetime recurrence rate is higher in males, although the incidence of nephrolithiasis is growing among females [18]. Therefore, prophylactic management is of great importance to manage urolithiasis.
Recent studies have reported that the prevalence of urolithiasis has been increasing in the past decades in both developed and developing countries. This growing trend is believed to be associated with changes in lifestyle modifications such as lack of physical activity and dietary habits [19–21] and global warming [16]. In the United States, kidney stone affects 1 in 11 people [22], and it is estimated that 600,000 Americans suffer from urinary stones every year. In Indian population, about 12% of them are expected to have urinary stones and out of which 50% may end up with loss of kidney functions [23].
2. The Urinary System and Stones
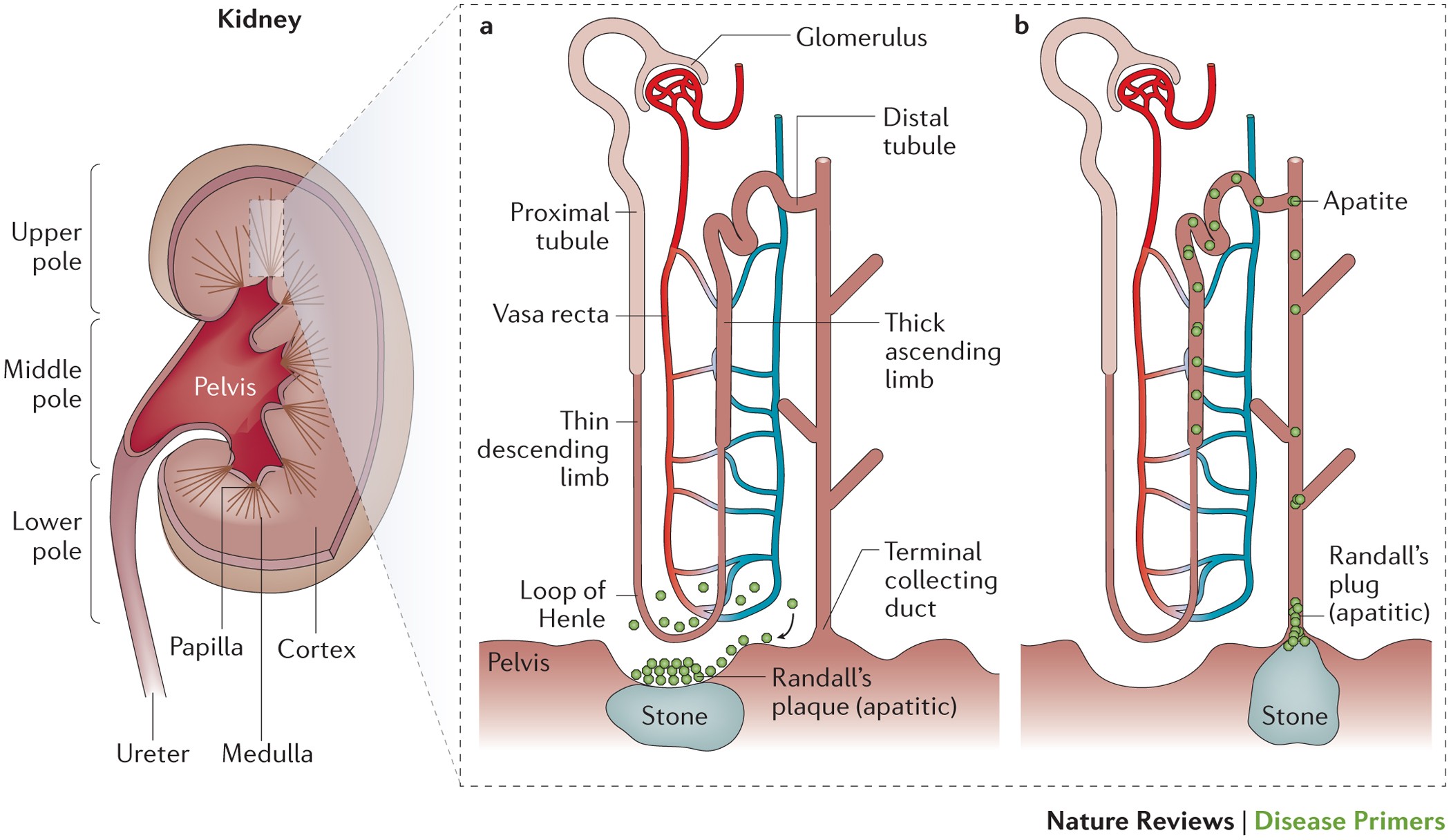
The urinary filtrate is formed in the glomerulus and passes into the tubules where the volume and content are altered by reabsorption or secretions. Most solute reabsorption occurs in the proximal tubules, whereas fine adjustments to urine composition take place in the distal tubule and collecting ducts. The loop of Henle serves to concentrate urine composed of 95% water, 2.5% urea, 2.5% mixture of minerals, salts, hormones, and enzymes. In the proximal tubules, glucose, sodium, chloride, and water are reabsorbed and returned to the blood stream along with essential nutrients such as amino acids, proteins, bicarbonate, calcium, phosphate, and potassium. In the distal tubule, the salt and acid-base balance of blood is regulated [24]. The location of stones may vary as indicated in Figure 1.
Kidney stone locations in the urinary system. (a) Adopted from [25]. (b) Adopted from [26].
3. Types of Kidney Stones
The chemical composition of kidney stones depends on the abnormalities in urine composition of various chemicals. Stones differ in size, shape, and chemical compositions (mineralogy) [27]. Based on variations in mineral composition and pathogenesis, kidney stones are commonly classified into five types as follows [28].
3.1. Calcium Stones: Calcium Oxalate and Calcium Phosphate
Calcium stones are predominant renal stones comprising about 80% of all urinary calculi [29]. The proportion of calcium stones may account for pure calcium oxalate (CaOx) (50%), calcium phosphate (CaP, termed as apatite) (5%), and a mixture of both (45%) [30]. The main constituent of calcium stones is brushite (calcium hydrogen phosphate) or hydroxyapatite [31, 32]. Calcium oxalate is found in the majority of kidney stones and exists in the form of CaOx monohydrate (COM, termed as mineral names: whewellite, CaC2O4·H2O), and CaOx dihydrate (COD, weddellite, CaC2O4·2H2O), or as a combination of both which accounts for greater than 60% [33]. COM is the most thermodynamically stable form of stone. COM is more frequently observed than COD in clinical stones [34].
Many factors contribute to CaOx stone formation such as hypercalciuria (resorptive, renal leak, absorptive, and metabolic diseases), hyperuricosuria, hyperoxaluria, hypocitraturia, hypomagnesuria, and hypercystinuria [35]. Mostly, urinary pH of 5.0 to 6.5 promotes CaOx stones [36], whereas calcium phosphate stones occur when pH is greater than 7.5 [11]. The recurrence of calcium stone is greater than other types of kidney stones.
3.2. Struvite or Magnesium Ammonium Phosphate Stones
Struvite stones occur to the extent of 10–15% and have also been referred to as infection stones and triple phosphate stones. It occurs among patients with chronic urinary tract infections that produce urease, the most common being Proteus mirabilis and less common pathogens include Klebsiella pneumonia, Pseudomonas aeruginosa, and Enterobacter [1, 28, 29]. Urease is necessary to split/cleave urea to ammonia and CO2, making urine more alkaline which elevates pH (typically > 7). Phosphate is less soluble at alkaline versus acidic pH, so phosphate precipitates on to the insoluble ammonium products, yielding to a large staghorn stone formation [37]. Women’s are likely to develop this type of stone than the male. Escherichia coli is not capable of splitting urea and is not associated with struvite stones [38].
3.3. Uric Acid Stones or Urate
This accounts approximately for 3–10% of all stone types [1, 29]. Diets high in purines especially those containing animal protein diet such as meat and fish, results in hyperuricosuria, low urine volume, and low urinary pH (pH < 5.05) exacerbates uric acid stone formation [11, 28, 39]. Peoples with gouty arthritis may form stones in the kidney(s). The most prevalent cause of uric acid nephrolithiasis is idiopathic [38], and uric acid stones are more common in men than in women.
3.4. Cystine Stones
These stones comprise less than 2% of all stone types. It is a genetic disorder of the transport of an amino acid and cystine. It results in an excess of cystinuria in urinary excretions [1, 29], which is an autosomal recessive disorder caused by a defect in the rBAT gene on chromosome 2 [40], resulting in impaired renal tubular absorption of cystine or leaking cystine into urine. It does not dissolve in urine and leads to cystine stone formation [11]. People who are homozygous for cystinuria excrete more than 600 millimole insoluble cystine per day [28]. The development of urinary cystine is the only clinical manifestation of this cystine stone disease [40].
3.5. Drug-Induced Stones
This accounts for about 1% of all stone types . Drugs such as guaifenesin, triamterene, atazanavir, and sulfa drugs induce these stones. For instance, people who take the protease inhibitor indinavir sulphate, a drug used to treat HIV infection, are at risk of developing kidney stones [28]. Such lithogenic drugs or its metabolites may deposit to form a nidus or on renal calculi already present. On the other hand, these drugs may induce the formation of calculi through its metabolic action by interfering with calcium oxalate or purine metabolisms [38].
4. Kidney Stone Compositions
The chemical compositions of urinary stones include crystals and noncrystalline phases or the organic material (the matrix). The organic matrix of urinary stones consists of macromolecules such as glycosaminoglycans (GAG’s), lipids, carbohydrates, and proteins. These molecules play a significant role by promoting or inhibiting the processes of kidney stone development (Table 1). The main components of the stone matrix are proteins (64%), nonamino sugars (9.6%), hexosamine as glucosamine (5%), water (10%), and inorganic ash (10.4%). The matrix acts as a template participating in the assembly of kidney stones. The matrix of all stones contains phospholipids (8.6%) of the total lipid, which in turn represents about 10.3% of stone matrix. Cell membrane phospholipids, as part of organic matrix, promote the formation of calcium oxalate and calcium phosphate stones [41]. Albumin is the major component of the matrix of all
I: inhibitor; P: promoter; “—”: no effect.
Brushite stone is a hard phosphate mineral with an increasing incidence rate, and a quarter of calcium phosphate (CaP) patients form stones containing brushite [43]. In the urinary tract, CaP may be present in the form of hydroxyapatite, carbonate apatite, or brushite (calcium monohydrogen phosphate dihydrate, CaHPO4·2H2O). Brushite is resistant to shock wave and ultrasonic lithotripsy treatment [44].
4.1. Etiology of Kidney Stones
Formation of kidney stones (calculogenesis) is a complex and multifactorial process including intrinsic (such as age, sex, and heredity) and extrinsic factors such as geography, climate, dietary, mineral composition, and water intake [15]. A summary of possible causes of kidney stone formation
5. Mechanisms of Renal Stone Formation
The pathogenesis of kidney stone or biomineralization is a complex biochemical process which remains incompletely understood [41]. Renal stone formation is a biological process that involves physicochemical changes and supersaturation of urine. Supersaturated solution refers to a solution that contains more of dissolved material than could be dissolved by the solvent under normal circumstances [34]. As a result of supersaturation, solutes precipitate in urine leads to nucleation and then crystal concretions are formed. That is, crystallization occurs when the concentration of two ions exceeds their saturation point in the solution [55]. The transformation of a liquid to a solid phase is influenced by pH and specific concentrations of excess substances. The level of urinary saturation with respect to the stone-forming constituents like calcium, phosphorus, uric acid, oxalate, cystine, and low urine volume are risk factors for crystallization [1, 56]. Thus, crystallization process depends on the thermodynamics (that leads to nucleation) and kinetics (which comprises the rates of nucleation or crystal growth) of a supersaturated solution [57]. Therefore, lithiasis can be prevented by avoiding supersaturation.
However, it should be noted that stone formation is usually dependent on the level of imbalance between urinary inhibitors and promoters of crystallization. All stones share similar events with respect to the mineral phase of stone formation. But, the sequence of events leading to stone formation differs depending on the type of stone and urine chemistry. For instance, crystallization of calcium-based stones (calcium oxalate or calcium phosphate) occurs in supersaturated urine if it is with low concentrations of inhibitors. Uric acid interferes the solubility of calcium oxalate and promotes CaOx stone formation. In healthy controls, crystallization process is opposed by inhibitory substances and gets safe [1]. The sequence of events that trigger stone formation includes nucleation, growth, aggregation, and retention of crystals within the kidneys [27, 58].
5.1. Crystal Nucleation
The first step in the formation of kidney stone begins by the formation of nucleus (termed as nidus) from supersaturated urine retained inside the kidneys [11, 42]. In a supersaturated liquid, free atoms, ions, or molecules start forming microscopic clusters that precipitate when the bulk free energy of the cluster is less than that of the liquid. For example, charged soluble molecules such as calcium and oxalate combine to form calcium oxalate crystals and become insoluble [34]. Nucleation may be formed in the kidney through free particle or fixed particle mechanism [26, 34]. In supersaturated solutions, if promoters exceed that of inhibitors, nucleation starts [34].
Once a nucleus is created (and/or if it is anchored), crystallization can occur at lower chemical pressure than required for the formation of the initial nucleus. Existing epithelial cells, urinary casts, RBCs, and other crystals in urine can act as nucleating centers in the process of nuclei formation termed as heterogeneous nucleation [41]. The organic matrix, mucopolysaccharide acts as a binding agent by increasing heterogeneous nucleation and crystal aggregation [59]. On the other hand, nanobacteria is claimed to form apatite structures serving as a crystallization center for stone formation [60]. The whole process potentiates stone formation. The role of oxalate-degrading bacteria, such as Oxalobacter formigenes, in CaOx stone formation is a subject of current research [61]. Thus, treatment which targets the process of nucleation intervention is one of the best approaches to control kidney stone.
5.2. Crystal Growth
Crystals in urine stick together to form a small hard mass of stone referred as crystal growth. Stone growth is accomplished through aggregation of preformed crystals or secondary nucleation of crystal on the matrix-coated surface [62]. Once a nidus has achieved, the overall free energy is decreased by adding new crystal components to its surface. The total free energy of the cluster is increased by the surface energy. The process of stone growth is slow and requires longer time to obstruct the renal tubules [34]. From organic matrix, mainly Tamm–Horsfall protein and osteopontin are promoters of CaOx stone formation [13]. Under in vitro study, crystals induced in human urine demonstrated an intimate association between calcium-containing crystals and organic matrix (lipids and proteins). Lipids of cellular membranes are basically believed to involve in nucleation of crystals [63].
5.3. Crystal Aggregation
The process whereby a small hard mass of a crystal in solution sticks together to form a larger stone is called aggregation. All models of CaOx urolithiasis concede that crystal aggregation is probably involved in crystal retention within the kidneys [41]. Crystal aggregation is considered to be the most critical step in stone formation.
5.4. Crystal-Cell Interaction
The attachment of grown crystals with the renal tubule lining of epithelial cells is termed as crystal retention or crystal-cell interaction [41, 64]. In individuals with hyperoxaluria, renal tubular epithelial cells were injured due to exposure to high oxalate concentrations or sharp calcium oxalate monohydrate (COM) crystals [10, 65, 66]. Crystal-cell interaction results in the movement of crystals from basolateral side of cells to the basement membrane [10]. Then, crystals could be taken into cells and anchored to the basement membrane of the kidneys [66]. The interaction of COM crystals with the surface of renal epithelial cells could be a critical initiating event in nephrolithiasis. An increased retention force between the crystal and injured renal tubule epithelium cells promotes CaOx crystallization [67]. Most of the crystals attached to epithelial cells are thought to be digested by macrophages and/or lysosomes inside cells and then discharged with urine [66].
Following renal tubular cell injury, cellular degradation produces numerous membrane vesicles which are nucleators of calcium crystals as supported by in vitro and in vivo studies [41]. Injured cells release substances like renal prothrombin fragment-1 or other anionic proteins which induce COM crystal agglomeration [68]. Reactive oxygen species is thought to be one of the factors involved in renal cell injury [69]. Thus, reduction of renal oxidative stress could be an effective treatment option.
Injured cells potentiate to invert its cell membrane which is anionic to the urinary environment and acts as site of crystal adherence. COM crystals have stronger affinity of attachment towards the inverted anionic membrane [69], than calcium oxalate dihydrate (COD) crystals [70]. On the other hand, deposition of COM crystal was observed in Madin–Darby canine kidney epithelial cells (MDCK cells), than at proximal tubular epithelial cells derived from pig kidney (LLC-PK1 cells) study models [71]. This preferential difference may be due to the presence of a binding molecule such as hyaluronan on Madin–Darby canine kidney epithelial cells for COM crystal attachment [67]. Although the detailed mechanisms of crystal-cell interaction remain unexplored, one of the best ways to treat urolithiasis is to control crystal-cell retentions.
5.5. Endocytosis of CaOx Crystals
Endocytosis or engulfment of crystals by renal tubular cells is the earliest process in the formation of kidney stones. Studies on tissue culture crystal-cell interactions indicated that COM crystals rapidly adhere to microvilli on the cell surface and subsequently internalized. Polyanion molecules present in tubular fluid/urine such as glycosaminoglycans, glycoproteins, and citrate may coat crystals and inhibit the binding of COM crystals to cell membrane [41]. For example, Tamm–Horsfall glycoproteins (THP) have a dual biological role in stone formation. Lieske et al. [72] reported that THP may promote renal stone formation by initiating the interaction of COM crystals with distal tubular cells of the nephron. Another study revealed that, upon lowering pH and raising ionic strength, THP’s viscosity increases which exhibits high tendency of polymerization and fails to inhibit crystallization. Moreover, THP becomes a strong promoter of crystallization in the presence of additional calcium ions [73]. In contrast, THP is thought to protect against COM stone formation by inhibiting COM aggregation when it is at high pH and low ionic strength as reported by Hess [73]. COM aggregation assays revealed that desialylated THP promoted COM aggregation, while normal THP inhibited aggregation [74]. Similar reports revealed that THP may inhibit calcium oxalate crystal aggregation, whereas uromodulin may promote aggregation [75]. Inactivating the THP gene in mouse embryonic stem cells results in spontaneous formation of calcium crystals in adult kidneys. This is a convincing evidence that THP is a critical urinary inhibitor of human nephrolithiasis [76].
Various cellular and extracellular events are involved during stone formation. Modulators targeting the steps from supersaturation to crystal retention may be a potential means to block stone formation. Similarly, the blockage of crystal binding molecules (such as osteopontin, hyaluronic acid, sialic acid, and monocyte chemoattractant protein-1) expressed on epithelial cell membranes may be an alternative approach to prevent stone formation [41]. Experimental findings demonstrated that stone calcification is triggered by reactive oxygen species (ROS) and the development of oxidative stress [77]. In vitro [78, 79] and in vivo [80, 81] studies have demonstrated that CaOx crystals are toxic for renal epithelial cells that produce injury and renal cell death. Similarly, an exposure to hypercalciuria produces cellular injury and ROS-induced lipid peroxidation which stimulates calcium oxalate deposition [82]. The pathophysiology of urinary stone formation is incompletely understood. A summary of the various steps involved in stone formation